Protecting access to healthcare during COVID-19 and beyond
Healthcare providers have been overwhelmed by the demand for COVID-19-related care. Medical appointments and treatments for other conditions have often been delayed, potentially leading to escalating health problems and greater future care needs among those who have missed out. If the pandemic leads to an economic crash, this rise in unmet medical needs could spiral, as happened during the last economic crisis – policymakers should take heed.
Fall-off in services
Between March and July 2020, over one-fifth of people in the EU who needed a medical examination or medical treatment did not receive it. When asked why, 9 out of 10 gave a COVID-19-related reason. For the vast majority, lack of availability due to COVID-19 was a problem, with 85% of respondents giving this reason to Eurofound’s Living, working and COVID-19 survey, as the figure below shows. The percentage was similar across Member States. In that period, healthcare institutions throughout Europe cancelled or postponed services for non-COVID patients, to deal with the huge numbers of patients infected with the Coronavirus and in need of urgent care.
Figure 1: Reasons for unmet medical needs since the onset of the COVID-19 pandemic (%), EU27, July 2020
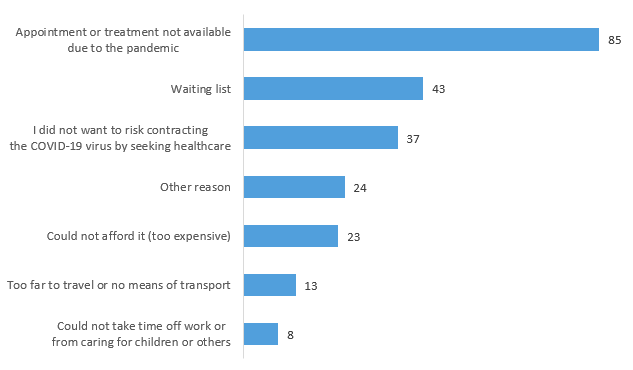
Note: Respondents assessed all reasons on a scale of 1 to 5 where 1 is ‘not at all important’ and 5 is ‘very important’; the percentages who indicated 4 and 5 are shown.
Source: Eurofound, Living, working and COVID-19 survey, second round (July 2020)
The other COVID-19-related reason for unmet needs was fear of contracting the disease, given by 37% of respondents. The percentage was much higher in some Member States, particularly Bulgaria, Greece and Sweden, where it was around 60%. This could reflect a lack of trust that services were sufficiently well-prepared to protect people from the virus.
The COVID-19 pandemic thus added a massive new layer to the access problems that people already experience when they need medical attention. Still, traditional problems such as waiting lists (sometimes caused by the pandemic), distance from services and unaffordability remained prevalent.
Even countries that have traditionally had low levels of unmet medical needs have seen these rocket during the pandemic. For example, Spain has consistently been one of the most effective Member States in responding to its population’s healthcare needs, but the gravity of the pandemic there meant that nearly a quarter of people reported unmet needs between March and July, higher than the EU average.
Publication: Living, working and COVID-19
More unmet needs to come
Before the COVID-19 pandemic, unmet medical needs had been steadily decreasing since peaking in 2014–2015 following the 2007–2008 global financial crisis. Interestingly, that peak was reached after that crisis had passed, likely due to the delayed impact of austerity measures implemented towards the end of the crisis, which led to hiring freezes and increased co-payments by service recipients. This time, the impact of an economic crisis could be more immediate if policymakers fail to take appropriate action.
Important drivers of improved access to healthcare in recent years have been rises in people’s income and increased employment. As a result, more people were able to afford medical fees or supplementary health insurance, or were given such insurance through their employment, ensuring timely access to good quality care. These income- and employment-driven decreases in unmet needs were not accompanied by a broad improvement in access for all, which could have been achieved in part by reversing some of the austerity measures that had been implemented.
The reliance on income and employment as a means of improving access to healthcare means that challenges arise as soon as an economic downturn strikes. Already in July 2020, 7.9% of people in the EU reported that their households had been unable to make scheduled payments related to healthcare and health insurance, up from 6.5% three months earlier.
Being unable to pay for healthcare often means not getting healthcare – evidenced by the finding that 44% of people with healthcare or health insurance arrears have unmet needs, compared to 19% of people without such arrears. Healthcare or health insurance arrears are particularly common among unemployed people, and the proportion with such arrears rose dramatically between March and July 2020 (Figure 2). It is concerning that, of those who lost their job during the pandemic, 32% reported in July that they had had unmet medical needs since the start of the pandemic, compared to 21% of people who had not become unemployed.
Figure 2 : Healthcare or health insurance arrears among different population groups (%), EU27, April and July 2020
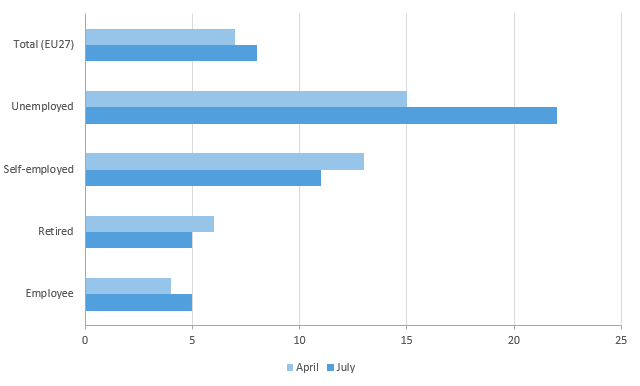
Source: Eurofound, Living, working and COVID-19 survey, first and second rounds (April and July 2020)
Similarly, people who say they have great difficulty making ends meet are almost three times more likely to have experienced unmet medical needs for any reason (33%) than people who make ends meet easily (12%). In the EU, however, many people with limited financial means do manage to get the healthcare they require because Member States have put mechanisms in place to guarantee some level of access. For instance, in Ireland, many people who saw their income decline during the 2007–2008 global financial crisis became instantly entitled to a medical card, guaranteeing access to free basic healthcare. In some countries (such as Austria and Spain) there is little difference between income groups in meeting their medical needs. However, overall, current state interventions have proved insufficient to prevent an ‘affluence gap’ in accessing healthcare.
Publication: Access to care services: Early childhood education and care, healthcare and long-term care
Safeguarding access in downturns
Policymakers need to take action to prevent the current deterioration in access to healthcare – due mainly to unavailability of care – from being exacerbated if there is a pandemic-driven recession. This could be done by making healthcare access less dependent on income and employment. The COVID-19 public health crisis has highlighted the importance of investing in prevention and healthcare, and the policy reaction to the COVID-19 crisis has so far been fundamentally different from the austerity-based approach in the previous crisis. However, sustained policy attention is needed to ensure access for all and to safeguard access when the economy contracts.
A larger role could be played by e-healthcare, which could put many services within closer reach. E-consultations and e-prescriptions were facilitated widely during the first wave of the pandemic. This was a great leap forward, given the slow progress made by many Member States up until then. However, efforts should be made to consolidate such, often temporary, solutions and to develop robust e-healthcare structures. Some Member States have made big strides. In France, for instance, screen-to-screen consultations with GPs and specialists are available nationwide and can take place in a pharmacy if medical equipment is needed. Estonia has a national healthcare telephone line staffed by experienced GPs and nurses, with almost 9 out of 10 callers’ needs addressed without a follow-up face-to-face meeting.
Image © goodluz/Adobe Stock
Authors
Hans Dubois
Senior research managerHans Dubois is a senior research manager in the Social Policies unit at Eurofound. His research topics include housing, over-indebtedness, healthcare, long-term care, social benefits, retirement, and quality of life in the local area. Prior to joining Eurofound, he was Assistant Professor at Kozminski University (Warsaw). He completed a PhD in Business Administration and Management at Bocconi University (Milan), after working as a research officer at the European Observatory on Health Systems and Policies (Madrid).
Tadas Leončikas
Head of UnitTadas Leončikas is Head of the Employment unit at Eurofound since September 2022. Prior to this, he was a senior research manager in the Social Policies unit, managing the European Quality of Life Survey (EQLS) and developing Eurofound's survey research. Since joining Eurofound in 2010, he has worked on various topics including survey methods, quality of life, social mobility, social inclusion, trust and housing inadequacies. In his earlier career, he headed up the Institute for Ethnic Studies in Lithuania where he worked on studies related to the situation of ethnic minorities, migrants and other vulnerable groups. As a researcher, he has previously collaborated with the European Union Agency for Fundamental Rights, the United Nations Development Programme and the International Organization for Migration. He has a PhD in Sociology.
Related content
8 October 2020
The right of access to good-quality care services is highlighted in the European Pillar of Social Rights. This report focuses on three care services: early childhood education and care (ECEC), healthcare, and long-term care. Access to these services has been shown to contribute to reducing inequalities throughout the life cycle and achieving equality for women and persons with disabilities. Drawing on input from the Network of Eurofound Correspondents and Eurofound’s own research, the report presents an overview of the current situation in various EU Member States, Norway and the UK, outlining barriers to the take-up of care services and differences in access issues between population groups. It pays particular attention to three areas that have the potential to improve access to services: ECEC for children with disabilities and special educational needs, e-healthcare and respite care.
27 September 2020
This report presents the findings of the Living, working and COVID-19 e-survey, carried out by Eurofound to capture the far-reaching implications of the pandemic for the way people live and work across Europe. The survey was fielded online, among respondents who were reached via Eurofound’s stakeholders and social media advertising. Two rounds of the e-survey have been carried out to date: one in April, when most Member States were in lockdown, and one in July, when society and economies were slowly re-opening.
The findings of the e-survey from the first round reflected widespread emotional distress, financial concern and low levels of trust in institutions. Levels of concern abated somewhat in the second round, particularly among groups of respondents who were benefiting from support measures implemented during the pandemic. At the same time, the results underline stark differences between countries and between socioeconomic groups that point to growing inequalities.
The results confirm the upsurge in teleworking across all countries during the COVID-19 pandemic that has been documented elsewhere, and the report explores what this means for work–life balance and elements of job quality.
